As a mass disease in the USSR, the main requirements for prevention in our country are early detection and treatment of patients, as well as control of the vector. For early detection of patients and parasite carriers, it is necessary to test the blood for malaria in all febrile patients arriving from malaria-prone areas and from abroad. To combat and exterminate larvae, larvicides are used (see), to exterminate winged mosquitoes - persistent insecticides (DDT, hexachlorane, chlorophos, etc.), repellents (see). When entering malaria-endemic areas, individual chemoprophylaxis is carried out. Take 4-aminoquinoline derivatives (chloroquine, resokhin, etc.) 0.5 g once a week while staying in an endemic focus and for 4 weeks after leaving it. Those who have recovered from malaria are subject to dispensary observation for two years.
Prevention . For individual chemoprophylaxis of malaria, take 4-aminoquinoline drugs (chingamin, chloroquine, resoquine, etc.) at a dose of 0.3 g of base per day, 2 days a week (in a row or at intervals of 1-3 days), a total of 0.6 g. Bigumal can also be prescribed at 0.3 e for 2 days a week. Taking medications begins 2 weeks before arriving at the malaria outbreak and continues for 3-4 weeks after leaving it. Since chemoprophylaxis does not provide a cure for malaria, a course of treatment is recommended after leaving hyperendemic foci of malaria.
In the recent past, the fight against malaria was practically aimed only at reducing the incidence. At the same time, labor-intensive and expensive, but ineffective measures were carried out annually to exterminate the vector. Bonification (cleaning reservoirs of vegetation and sediment, liquidation of small reservoirs of no economic importance), reclamation (regulation of the water regime of the area - construction of drainage canals, drainage, etc.), oiling, treatment of Parisian greens, etc. anophelogenic reservoirs for the release them from mosquito larvae (delavation) only provided some success for a relatively short time and in limited areas.
From 1944-1945 To exterminate winged mosquitoes of the genus Anopheles, they began to spray premises (residential and commercial buildings) with persistent insecticides (DDT, hexachlorane, chlorophos, etc.). The use of persistent insecticides shortens the lifespan of female mosquitoes so much that they do not survive until sporozoites can appear in their salivary glands. This leads to the cessation of transmission of infection. The practical significance of persistent insecticides in the fight against winged mosquitoes of the genus Anopheles lies in their high epidemiological effectiveness, comparative cheapness and low labor intensity. The premises are treated 1-2 times a season, DDT consumption is 1-2 g/m2. The extermination of winged mosquitoes by insecticides with a long residual effect is superior in epidemiological effectiveness to any of the known antimalarial measures.
In 1953, the WHO expert committee on malaria spoke in favor of the feasibility of eliminating malaria throughout the world, and in 1955, the 8th WHO Assembly adopted a special decision on this issue. The malaria eradication program has four phases: preparatory, attack, consolidation and maintenance. The preparatory phase should not last more than a year; At this time, the epidemiological situation is clarified, an action plan is developed, personnel, equipment, and transport are recruited and prepared. Then the attack phase begins, it usually lasts 3-4 years, during which the premises are completely processed. They move to the consolidation phase when the incidence of malaria in the protected territory does not exceed 5 cases per 10,000 population; it lasts 3 years, during which residual foci of malaria are eliminated, epidemiological surveillance and blood testing of the population are organized (at least 10% in the most previously affected areas). If no new local cases of malaria are identified, the maintenance phase begins; it does not require special staff and is carried out by the existing medical network. Treatment of patients with malaria is carried out at all phases. Massive administration of medications (chemoprophylaxis) is used when indicated. Larvicidal measures are limited to areas where indoor treatment is not effective enough.
A shortcoming of the WHO malaria eradication program is the known underestimation of efforts to actively identify patients and treat them; this makes implementation of the program difficult.
The first mention in European literature of the treatment of intermittent fevers with an extract from the bark of the cinchona tree dates back to 1643. In 1820, the French chemists P. J. Pelletier and J. B. Caventou isolated the alkaloid quinine in its pure form. Schuleman, Schonhofer, and Wingler produced the first synthetic antimalarial drug, plasmochin, in 1926. In 1931, O. Yu. Magidson, I. T. Strukov, G. V. Chelintsev and I. L. Knunyants synthesized plasmocide, in 1933 I. L. Knunyants, G. V. Chelintsev, A. Malaria Grigorovsky and S. V. Benevolenskaya - Akrikhin.
In 1939, the Swiss P. N. Muller discovered the insecticidal effect of DDT, synthesized in 1874, which made it possible to begin work on combating the malaria vector. In 1944, paludrin was synthesized in England, in 1945 in the USA - the first of 4 aminoquinoline derivatives - chloroquine.
Distribution and statistics
The ancient primary focus of Malaria is considered to be tropical Africa, from where the disease spread to India, China and Indochina, and through the Nile Valley to Mesopotamia and the Mediterranean countries. According to V.V. Favre, malaria was brought to Russia from Iran.
The northern limit of the Malaria range reached 49° north latitude in North America and 64° north latitude in Europe and Asia; the southern border reached 33° south latitude in South America, 31° south latitude in Africa and 20° south latitude in Australia. Within these boundaries, Malaria was absent in high mountain and desert areas, on a number of islands in the Pacific and Atlantic Oceans, not inhabited by Anopheles mosquitoes. The highest located foci of Malaria were recorded at an altitude of 3500 m above sea level North of 49-64° north latitude and south of 33-20° south latitude, transmission of Malaria does not occur due to lack of heat for the development of plasmodium in the mosquito body.
P. falciparum has not been found to have adaptive properties for existence outside a hot climate zone. With a significant import of tropical malaria, outbreaks occurred in some hot years at latitudes such as 61° north latitude (the city of Solvychegodsk, USSR), and at such altitudes as 2590 meters above sea level (Kenya). The stable boundary of the range of P. falciparum in the northern hemisphere was at 45-50° north latitude, in the southern hemisphere - at 20° south latitude
The range of P. malariae is limited to 53°N latitude (Netherlands) and 29°S latitude (Argentina). Characterized by pronounced nesting of foci of four-day malaria; In many areas where tertian and tropical malaria are endemic, quaternary malaria is absent.
Malaria had a huge impact on the lives of many peoples. Thus, by the beginning of the 30s of the 20th century, about 700 million people in the world fell ill with malaria every year, of whom about 7 million died
The targeted fight against malaria, carried out in the 20th century in many countries of the world and especially in the USSR, significantly changed the situation.
Back in 1921, mandatory registration of patients with Malaria was introduced in the RSFSR. In subsequent years, the task was set to significantly reduce the incidence of Malaria, suppress outbreaks of the disease, and reduce disability as a result of Malaria. This was achieved by a complex of antimalarial measures developed by Soviet scientists (E. I. Martsinovsky and others) and carried out by Soviet health authorities.
In 1949, the USSR set the task of eliminating malaria as a mass disease (reducing the intensive incidence rate of malaria below 10 per 10,000 population). The high efficiency of methods of combating Malaria (Figure 1), in particular the effective treatment of patients, the use of persistent contact insecticides to combat winged Anopheles, made it possible to achieve the elimination of Malaria as a mass disease throughout the USSR by 1952 (intensive incidence rate of Malaria 9.8 per 10,000 population).
Great changes in the incidence of malaria have occurred throughout the world during the implementation of the global program of its elimination, which began in 1955 under the auspices of WHO. In the first 10 years (1956-1965), significant progress was made on all continents except Africa. Vast malaria-free zones have appeared in Europe, India, the USA, the Caribbean islands, Mexico, and Venezuela.
Subsequently, the process of eliminating malaria slowed down and finally practically stopped. In the 70s, malaria diseases were again observed in previously healthy areas of Iran, Iraq, Turkey and Syria. Malaria has become a major health problem in India, Sri Lanka and Burma; its incidence has increased sharply in Thailand, the Philippines, and a number of countries in Central and South America. In the territories of Europe, North America and Japan, which have been cleared of malaria, the number of imported cases of malaria has increased. This was accompanied by the development of outbreaks of the disease, an increase in mortality and an increase in vaccine-induced malaria.
The number of malaria cases in the world in 1976 was 150 million people. Tropical malaria accounts for 50% of all cases of disease, three-day malaria - 43% and four-day malaria - 7%. In Africa (the world “epicenter” of Malaria), according to incomplete data, from 2 to 17 thousand diseases per 100,000 inhabitants are registered annually. In a number of countries in tropical Africa, malaria diseases account for an average of over 12% of the total morbidity.
The mortality rate directly associated with malaria is approximately 1%. More than 1 million people a year die from malaria, mainly in tropical Africa. During catastrophic epidemic surges, the mortality rate for malaria reached 3-5%, in some areas and settlements - 20-40%. P. falciparum is the cause of 98% of all deaths from malaria. In the 60-70s, the highest mortality from tropical malaria was observed in Europe and the USA; for the period 1967-1972 it was 2.7% in Europe (in the UK in 1970-1973 - 5.2%), in the USA - 8.4%. This is due to the lack of immunity in the majority of patients and incorrect or delayed diagnosis of the disease.
The failures of the malaria eradication program in the world are associated with a number of factors: the inflation that has gripped the capitalist world, the reduction of financial support from developed capitalist countries, the shortage and rise in cost of insecticides, the emergence of resistance in vectors to insecticides and in malaria pathogens to drugs, an insufficient number of trained personnel and the poor state of health services in some countries.
Soviet citizens traveling to malaria-endemic countries are at risk of infection: in tropical Africa - mainly P. falciparum, less often P. ovale and P. malariae and very rarely P. vivax; in North Africa - P. vivax; in Asia - mainly P. vivax, less often P. falciparum (in Nepal and the Philippines - P. malariae); in Central and South America - mainly P. vivax, less often P. falciparum.
Etiology
The causative agents of Malaria are single-celled microorganisms belonging to the phylum Protozoa, class Sporozoa, order Haemosporidia, family Plasmodiidae, genus Plasmodium. There are 4 known types of human malaria pathogens: Plasmodium vivax (Grassi et Feletti, 1890) Labbe, 1899 - the causative agent of three-day malaria; Plasmodium malariae (Laveran, 1881) Grassi et Feletti, 1890 - causative agent of quartan malaria; Plasmodium falciparum Welch, 1897 - causative agent of tropical malaria; Plasmodium ovale Stephens, 1922 - the causative agent of ovale Malaria.
Malaria pathogens differ in a number of characteristics: virulence, resistance to the effects of chemotherapy drugs, duration of the incubation period, immunological characteristics, ability to infect mosquitoes, and others.
N.A. Sakharov in 1889 gave the first detailed description of the causative agent of tropical malaria, and in 1893 he described flagellar bodies as stages of development of malarial plasmodia. In 1890, D. Grassi and R. Feletti gave the first separate description of the causative agent of three-day malaria - P. vivax and the causative agent of four-day malaria - P. malariae. Welsh (W. N. Welch) in 1897 proposed the species name “falciparum” for the pathogen of tropical malaria. In 1922, J. W. W. Stephens proposed the name and described the morphology and development of P. ovale.
The pathogens of Malaria are characterized by a complex development cycle with a change of host (color figure 1). Asexual development (schizogony) occurs in the human body, sexual development (sporogony) occurs in the body of female mosquitoes of the genus Anopheles (see full body of knowledge Anopheles).
In the human body, two phases of development of malaria pathogens are distinguished: in liver cells - exoerythrocytic (extra-erythrocytic, tissue) schizogony and in erythrocytes - erythrocyte schizogony.
The erythrocyte membrane is invaginated at the site of attachment of the P. vivax merozoite only in cases where Duffy group isoantigens (Fya or Fyb) are present on the surface of the erythrocyte. The membrane of erythrocytes that do not have Duffy group isoantigens upon attachment of the P. vivax merozoite is not invaginated and erythrocyte schizogony does not occur. Such red blood cells are found very often among the aborigines of West Africa, as a result of which they are resistant to three-day malaria, although they are easily infected by other types of human plasmodium.
The duration of schizogony in P. vivax, P. ovale and P. falciparum is 2 days, in P. malariae - 3 days
The duration of gametocyte maturation (gametocytogony) in P. vivax, P. ovale and P. malariae is several hours longer than the duration of erythrocyte schizogony. Gametocytes of P. falciparum mature only after 10-12 days. Mature gametocytes do not undergo further changes in the human body and, if they do not enter the mosquito’s body, die: gametocytes of P. vivax, P. ovale and P. malariae - a few hours after reaching maturity , P. falciparum - a few weeks later.
The membrane of erythrocytes, in which the pathogens of Malaria are located at different stages of schizogony and gametocytogony in P. vivax, P. ovale and P. malariae, as well as ring-shaped trophozoites and gametocytes of P. falciparum, does not undergo changes. On the membrane of erythrocytes of subsequent (after ring-shaped trophozoites) stages of development of P. falciparum there is a protrusion that has an affinity for the endothelium of the capillaries of internal organs, where they are retained. Therefore, in peripheral blood it is usually possible to detect all stages of schizogony and gametocytogony of P. vivax, P. ovale and P. malariae and only ring-shaped trophozoites and gametocytes of P. falciparum.
Epidemiology
As a rule, in each country, zone, in a certain territory, there are 1-2 types of vectors, and in the whole globe - 25 - 30 types of vectors that determine the main incidence of Malaria. Some of the vectors of Malaria (A. gambiae, A. punctulatus, A. leucosphyrus, A. barbirostris, A. umbrosus) constitute the so-called species complexes. For example, the A. gambiae complex consists of 6 species that do not have absolute distinctive morphological (external) features and are identified only by their chromosome set. At the same time, the species included in the complex differ in behavior and ability to transmit malaria pathogens
The most effective vectors of malaria from the A. gambiae complex are considered to be A. funestus in tropical Africa and A. punctulatus in Papua New Guinea. These mosquitoes are highly sensitive to infection by Plasmodium Malaria in humans, a large percentage of them survive to an epidemically dangerous age (that is, until the appearance of sporozoites in the salivary glands), they are distinguished by a high degree of anthropophilicity (that is, they preferentially feed on human blood) and endophilicity (they attack humans mainly in residential areas). premises). The range of these vectors includes territories with the highest levels of malaria-holoendemic populations. Hyperendemic foci are created by A. darlingi and A. albimanus in South and Central America; A. fluviatilis, A. culicifacies, A. sundaicus, A. maculatus and A. minimus in Southeast Asia; A. labranchiae, A. sacharovi, A. sergenti, A. stephensi and A. superpictus in the Mediterranean, Near and Middle East. In the USSR, effective vectors of malaria include A. maculipennis (with subspecies), A. sacharovi, A. superpictus and A. pulcherrimus.
Depending on the social and natural conditions that promote or hinder the spread of malaria, a certain level of transmission intensity is established in each outbreak. In many countries with hot climates, this level remains unchanged for decades. As a result, foci of malaria arose and exist with a certain level of infestation (endemic level) and a characteristic immunological structure of the population.
The risk of contracting malaria in foci is determined depending on the type of endemic. The risk of infection characterizes the likelihood of a resident of a given outbreak being attacked by an infected mosquito. Holo and hyperendemic foci of Malaria have a high risk of infection, meso and hypoendemic foci have, respectively, an average and low risk of infection. The risk of infection initially inherent in a focus of this type can be significantly reduced by planned antimalarial measures. The structure of the Malaria area according to the risk of infection that had developed by 1972 is presented in Figure 3.
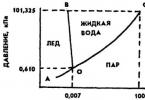
Among natural factors, the spread of malaria is influenced by climate, terrain and vegetation. Temperature conditions are of greatest importance in the development of the aquatic stages of Anopheles mosquitoes. The development of larvae of the most cold-resistant mosquito species is impossible at water temperatures below 10°. The temperature factor limits the spread of malaria pathogens, since the completion of the sporogony cycle in the body of the carrier occurs at a certain air temperature (table).
Air temperature also affects the duration of the gonotrophic cycle of mosquitoes, beginning with blood sucking and ending with egg laying. At high temperatures (from 25 to 30°), the duration of the gonotrophic cycle is 2 days; at lower levels - up to 7 days or more. During the period of sporogony, the female mosquito goes through several gonotrophic cycles. Physiologically old female mosquitoes, having completed several gonotrophic cycles, pose the greatest epidemiological danger, since the likelihood of them having sporozoites becomes especially high. The temperature conditions of sporogony also determine the intensity of infection of female mosquitoes with malarial plasmodia. At high temperatures, a larger number of oocysts and, consequently, sporozoites are formed.
Thus, in hot countries, the Malaria carrier more often feeds on humans, a relatively large part of its population survives to an infectious state and it is more intensively infected with the Malaria pathogen. All this is reflected in the epidemic process, the intensity of which in hot climate countries is tens and hundreds of times higher. than in temperate countries. In hot climates, precipitation affects the breeding site and the number of vectors, determining the geographic and seasonal distribution of Malaria. During the rainy season, mosquito breeding usually decreases or almost stops and their numbers drop sharply. With the help of wind, some mosquitoes (for example, A. pharoensis) can disperse tens and hundreds of kilometers from breeding sites and even cause outbreaks of malaria there
Transmission of Malaria decreases with increasing altitude and usually ceases at higher altitudes; In most mountainous areas there is no endemic malaria. The largest number of vector species at any latitude is confined to low and moderate altitudes of about 1000 meters above sea level. With increasing altitude, the fauna of Anopheles mosquitoes becomes depleted, and at very high altitudes their breeding is possible only in the tropical and subtropical zones, but even here it does not occur at altitudes above 3500 meters. The terrain determines the water flow system and thereby the presence, area and type of reservoirs suitable for colonization by Anopheles larvae, as well as human development of the territory.
Vegetation can become a natural barrier for malaria carriers, but under certain conditions it can also contribute to the breeding of mosquitoes.
Of the social factors, economic activity and human migration have the greatest influence on the formation of the malaria range. Destruction of forests, irrigation of new lands, construction of railways and highways, etc. led to the creation of a huge number of small bodies of water - breeding grounds for Anopheles mosquitoes, and the migrating population brought Malaria to areas previously free from this disease. Prof.'s conditions human activities that increase contact with the vector may cause a relatively greater spread of malaria in certain occupations. groups of people, mainly among people working near anophelogenic reservoirs, in the open air and at night.
Malaria epidemics can occur when an effective vector is introduced into an area where it was previously absent. Delivery by ship to the island. Mauritius A. gambiae and A. funestus caused a malaria epidemic in 1867-1868, during which 43 thousand deaths were recorded; The importation of A. gambiae from Africa to Brazil in the 1930s led to an epidemic of malaria, and out of 100 thousand people who fell ill, 14 thousand died.
Pathological anatomy
The forms of malaria caused by Plasmodium of different species, while having much in common, differ in some significant features.
A consequence of the increased functional load, as well as the irritating effect of decay products and foreign substances, is hyperplasia of the tissue elements of the spleen and liver with an increase in the size of these organs. With frequent relapses and lack of treatment, pulp sclerosis with dilation of the sinuses is observed. In the acute stages of invasion, the spleen tissue is very loose and full of blood, and the capsule is thin and tense. Organ ruptures are possible with minor trauma and even without clear reasons. Later, the capsule thickens, and the pulp becomes coarser, acquiring a dense, fleshy consistency, which persists even when the pigment completely disappears. The weight of the spleen can exceed 1 kilogram, occasionally reaching 5-6 kilograms or more.
A distinct enlargement of the liver is mainly due to hyperplasia of reticuloendothelial cells and plethora. In the future, fibrosis is possible - diffuse proliferation of fibrous connective tissue between the lobules and between hepatocytes, but the phenomena characteristic of typical liver cirrhosis are not observed.
Morphological changes in other organs and tissues during three-day malaria are less constant and are caused mainly by anemia, often reaching a very significant degree. One of the conditions that adversely affects blood regeneration is the property of P. vivax to settle predominantly in young red blood cells - reticulocytes.
The pathological anatomy of four-day malaria is basically similar to that of three-day malaria.
The accumulation of infected red blood cells in certain organs (with the exception of the brain), as a rule, does not cause significant damage. The cause of death in tropical malaria is most often damage to the central nervous system. Many researchers have observed that in patients who died from malarial coma, the capillary network of the brain is almost completely filled with red blood cells infected with the schizonts P. falciparum. The appearance of the brain and cerebellum of patients who died from a malarial coma is most characteristic when a deep loss of consciousness lasted about 24 hours. In such cases, the cortex, and partly the white matter of the brain, are brown-gray in color. The unusual coloring of the nervous tissue is clearly visible even in the early death of patients, but has a slightly different, sort of bluish tint. Along with the change in color, smoothing of the sulci and flattening of the gyri are noted, which indicates an increase in brain volume. Very often, pinpoint hemorrhages, sometimes numerous, are found in the brain matter. They arise mainly at the border between the cortex and the white matter of the hemispheres, in the internal capsules and in the corpus callosum, as well as in the cortex and the region of the dentate nuclei of the cerebellum.
The duration of the invasive process caused by P. falciparum in the human body rarely exceeds 1 year, caused by P. vivax and P. ovale - reaches 2 years, rarely 4-5 years, P. malariae - 2-3 years, sometimes tens of years. The incubation period depends on the type of pathogen. In tropical malaria, its duration is 6-31 days, in three-day malaria caused by P. vivax with short incubation - 7-21 days, caused by P. vivax with long incubation - 6-13 months, in oval malaria - 7-20 days, with a four-day period - 14-42 days. With inadequate chemoprophylaxis, the incubation period can increase significantly. Prodromal phenomena, sometimes observed during primary infection, are manifested by malaise, drowsiness, headache, low-grade fever, often followed by fever of the wrong type. After 3-4 days, a characteristic attack occurs, during which three clinical phases are distinguished: chills, fever, sweat. During the first phase, the patient experiences muscle pain, especially in the limbs and lower back, headache (see full body of knowledge), and sometimes vomiting. The skin becomes cold and bluish. The pulse quickens, breathing is shallow. The duration of chills is from 30-60 minutes to 2-3 hours or more. During the hot phase, which lasts from several hours to 1 day or more, the general condition worsens. The temperature reaches high numbers (40-41°), the face turns red, shortness of breath, agitation, and often vomiting appear. The headache gets worse. Sometimes delirium and a collapsed state occur. The amount of urine decreases (see full body of knowledge Oliguria). The end of the attack is determined by a decrease in temperature to normal and subnormal numbers and is accompanied by increased sweating (see full body of knowledge), lasting 2-5 hours. Then deep sleep sets in. In general, the attack lasts 6-10 hours, sometimes longer. Subsequently, for 1-2 days, depending on the type of pathogen, the normal temperature remains, but the patient experiences weakness, which increases after each attack. The attacks usually occur at the same time, but sometimes earlier or later. Often during the course of the disease, herpetic rashes appear (see Herpes), urticaria (see complete body of knowledge) or (in tropical malaria) hemorrhages, often in the form of petechiae (see full body of knowledge). After a series of attacks, the patient’s skin acquires a characteristic pale yellow tint. In severe cases of the disease, swelling may occur. After 3-4 attacks, the liver and spleen enlarge. Splenomegaly (see full body of knowledge) is an important diagnostic symptom, however, in severe cases of the disease, the size of the spleen remains normal. In persons aged 40-50 years, with any form of malaria, splenomegaly is less pronounced. With inadequate treatment and repeated infections, the spleen can reach large sizes (hypersplenism), anemia and leukopenia develop. Liver damage (see full body of knowledge), observed in most patients, is manifested by its enlargement, pain, often jaundice (see full body of knowledge), increased amount of direct bilirubin (see full body of knowledge Hyperbilirubinemia) and transaminase activity, decreased cholesterol (see full body of knowledge knowledge Hypocholesterolemia). Changes in the cardiovascular system (tachycardia, muffled heart sounds, hypotension, systolic murmur at the apex and base of the heart) are observed mainly during an attack. In severe forms, myocardial dystrophy develops in weakened and improperly treated patients (see full body of knowledge). Kidney damage most often manifests itself as febrile proteinuria, which is transient. In severe tropical malaria, as a rule, acute transient nephritis occurs with predominant damage to the tubules, and less often - chronic renal syndrome, etiologically associated with invasion of P. malaria. Disruption of the gastrointestinal tract during an attack is indicated by a decrease in appetite and stool upset, which disappear after the acute attacks of the disease are eliminated. Damage to the central nervous system is manifested by headache, especially intense in tropical malaria, nausea, and vomiting. At the height of attacks, febrile delirium, vegetative neuroses, and psychoses may occur. At altitude, and sometimes only at the end of the febrile period, leukopenia with neutropenia, relative lymphocytosis and monocytosis are detected in the blood. After several attacks, hemolytic anemia develops (see full body of knowledge Hemolytic anemia), polychromatophilia, and reticulocytosis. Without treatment, attacks can be repeated 10-12 times or more and stop spontaneously (but not with tropical malaria), but complete recovery does not occur. At the end of the latent period, which lasts from several weeks to 2-3 months, a period of relapses begins, which, in clinical manifestations, largely repeat the clinic of the primary attacks. Malaria in pregnant women takes a severe course, especially tropical malaria. Malignant forms often develop, accompanied by severe damage to the central nervous system, liver, kidneys, acute hemolysis, and disruption of pregnancy (miscarriages, premature birth, intrauterine fetal death). The consequence of inadequately treated malaria can be residual effects in the form of hyporegenerative anemia, splenomegaly, reaching a significant degree and accompanied by pancytopenia, vegetative neuroses. Three-day malaria in most cases is of moderate severity. In a typical course, attacks occur every other day (Figure 4, a), but there may also be a daily type of fever (Figure 4, 6). During the first 3-6 days, the temperature may be irregular or constant. Subsequently, the attack continues for 6-10 hours followed by apyrexia. Attacks usually occur in the morning. The end of the paroxysm is accompanied by profuse sweating. Three-day Malaria on the islands of the Western Pacific zone is characterized by a more severe course, characterized by frequent relapses and less sensitivity of pathogens to 8-aminoquinoline drugs. Four-day malaria is benign. Seizures occur after 2 days of apyrexia (Figure 4, c). Sometimes double attacks are observed - two days in a row followed by a period of apyrexia (one day), rarely daily. The attacks are longer than during three-day malaria, and their number is especially high in the absence of treatment. Frequent relapses are characteristic, and amyloid-lipoid nephrosis is possible. Tropical malaria is characterized by the most severe course, greater variability in clinical manifestations, but shorter duration. Characterized by an incorrect type of temperature curve (Figure 4, d). Chills are less pronounced and may be completely absent. Sweating is minor. In some cases, the fever takes on a three-day character, but the attacks are much longer (24-36 hours), and the periods of apyrexia are short. Severe headaches appear, often vomiting, diarrhea, jaundice, anemia quickly develops, and sometimes vestibular and cochlear lesions. Without timely treatment, tropical malaria can take a malignant course. Ovale malaria has a three-day course, but is milder. Attacks occur in the evening and at night. Spontaneous recovery is often observed.
DiagnosisWhen establishing a diagnosis, epidemiological, clinical and laboratory data are taken into account. With a typical course of the disease with the presence of characteristic attacks that occur with a clear frequency, accompanied by an enlargement of the liver and spleen, herpetic eruptions, and jaundice of the sclera, the diagnosis is beyond doubt. Indication of being in a malaria-endemic area makes the task easier. The detection of plasmodia in the blood (in a smear and thick drop) is crucial in the diagnosis. Research should be carried out in all cases of fever of unknown etiology, especially if there is an appropriate epidemiological history.
Serological tests are used to exclude the diagnosis of Malaria in patients with fever of unknown origin, hepatosplenomegaly, anemia, and when examining the blood of a donor from whom the recipient is believed to have become infected. They are also used as a method of epidemiological observation in areas that were previously unaffected by malaria. The presence of high titer antibodies in the blood serum of residents of non-endemic or malaria-free areas is evidence of malaria infection; in this regard, the patient should be questioned about his stay in an endemic area or the previous blood transfusion. Differential diagnosis. Some common clinical signs of Malaria (especially tropical Malaria) with dengue, phlebotomy fever, influenza, yellow fever, leptospirosis necessitate a differential diagnosis. It is necessary to take into account that dengue (see full body of knowledge) is characterized by a two-phase temperature curve, rash, joint and muscle pain, and changes in gait. Phlebotomy fever (see full body of knowledge) is characterized by intense pain in the spine, muscle pain in the lower extremities, sharp pain in the eyeballs when moving and in the upper eyelids when trying to lift them, injections of scleral vessels in the shape of a triangle in the outer corner of the eye. When making a differential diagnosis with influenza (see full body of knowledge), one should take into account the presence of catarrhal phenomena in the latter, hyperemia of the face and conjunctiva. Yellow fever (see full body of knowledge) in the initial phase is characterized by bright hyperemia of the skin and mucous membranes, pronounced bradycardia in the icteric phase, and a two-phase course of the disease. Leptospirosis (see full body of knowledge), unlike Malaria, is characterized by severe pain in the calf, occipital, and neck muscles, puffiness and hyperemia of the face and conjunctiva. Malarial coma is sometimes mistaken for overheating in the sun, alcohol intoxication, or meningoencephalitis. Correct diagnosis in this case can be helped by a detailed history (fever, poor health until a sudden deterioration in condition), data from a study of cerebrospinal fluid, which does not change in a malarial coma. In cases of malarial algid, cholera or salmonellosis may be suspected. The absence of dyspeptic symptoms at the onset of the disease and epidemiological anamnesis data exclude the latter. Sometimes it is necessary to differentiate Malaria from diseases such as cholecystitis, cholangitis, liver abscess, pyelonephritis, lymphogranulomatosis, which can be mistaken for Malaria
| ||||||||||||||||||||||||||
This order includes malarial plasmodia - the causative agents of malaria in reptiles, birds and many species of mammals. Four species are pathogenic for humans:
- Plasmodium vivax is the causative agent of tertian malaria,
- P. malariae is the causative agent of four-day malaria,
- P. falciparum is the causative agent of tropical malaria,
- P. ovale is the causative agent of tertian malaria.
These types of malarial plasmodia differ from each other in morphological and biological characteristics, the timing of development in the human body and the nature of the disease caused.
The definitive hosts of Plasmodium, the causative agent of human malaria, are mosquitoes of the genus Anopheles, which are called malarial mosquitoes; the intermediate host is humans.
Life cycle of malarial plasmodia using P. vivax as an example, is shown in Fig. 1.
- Tissue cycle - pre-erythrocytic schizogony
Human infection occurs as a result of the bite of an infected mosquito. Together with the saliva of an infected mosquito, plasmodia at the sporozoite stage enter the human blood. The sporozoites are carried throughout the body by the bloodstream and penetrate into the liver cells. In liver cells, they undergo the tissue (pre-erythrocytic) part of the development cycle: they acquire a rounded shape, grow, transform into the schizont stage and begin to divide through schizogony. From each schizont, many mononuclear tissue merozoites arise (1000-5000 individuals, depending on the type of plasmodium). The process of tissue development in P. falciparum lasts about 6 days, and in P. vivax - from 8 days to several months. The extra-erythrocyte part of the cycle corresponds to the main part of the incubation (latent) period of the disease. In all plasmodia pathogenic to humans, the preerythrocyte cycle occurs once.
When the liver cell is destroyed, some of the tissue merozoites again penetrate into the liver cells, where a new generation of tissue schizonts develops. Another part of tissue merozoites enters the bloodstream and penetrates into red blood cells. The erythrocyte part of the development cycle begins.
- Erythrocyte cycle - endoerythrocyte schizogony
Subsequently, the vacuole gradually decreases, the volume of the cytoplasm increases and pseudopodia are actively formed. The schizont grows rapidly due to the absorption of hemoglobin from the erythrocyte, releases pseudopodia and moves amoeboidally inside the erythrocyte. This gave rise to the name of one of the types of plasmodia P. vivax (i.e., living). This stage of development is called the amoeboid schizont.
After several cycles of asexual reproduction, preparation for the sexual process begins. Some merozoites, having penetrated erythrocytes, develop not into schizonts, but into sexual forms. From them gametocytes (immature sexual individuals) are formed, which differ morphologically from schizonts in their larger sizes, rounded shape and darker nucleus. There are females - macrogametocytes and males - microgametocytes. In the human body, reproduction and further development of gametocytes does not occur. Their further development is possible only in the body of a mosquito of the genus Anopheles, in which the process of sexual reproduction and sporogony occurs.
- Sexual reproduction and sporogony
Gametocytes enter the stomach of a female mosquito while feeding on the blood of a person with malaria. In the mosquito's stomach, they begin to develop, transforming from macrogametocytes into mature sexual forms, or macrogametes. During the process of maturation, the microgametocyte divides several times, forming 5-6 filamentous microgametes. The macrogametocyte increases in size and turns into a macrogamete. After fertilization, the resulting zygote acquires an elongated shape, becomes a mobile ookinete, passes through the wall of the mosquito’s stomach and stops in its outer layer, where it is covered with a membrane, greatly increases in size and is then called an oocyst. Then the process of sporogony begins, as a result of which, during the division of the nucleus and cytoplasm, a huge number of sporozoites (up to 10,000) are formed inside the oocyst. The shell of mature oocysts bursts, and the sporozoites penetrate all organs of the mosquito. The largest number of them accumulate in the salivary glands. When bitten, along with mosquito saliva, sporozoites enter the human bloodstream, which then penetrate into liver cells.
Thus, for humans the invasive stage is the sporozoite, and for the mosquito it is macro- and microgametocytes.
For the development of plasmodium in the mosquito's body, a certain minimum temperature is required. For P. vivax - not lower than 14.5 ° C, therefore, in areas with short and cold summers there are no local diseases of malaria.
Malaria is an anthroponotic protozoan disease with a vector-borne transmission mechanism.
In areas with a high level of endemicity, where the adult population has acquired immunity, the main source of infection is children.
The transmission mechanism of the pathogen is transmissible. The carrier is female mosquitoes of the genus Anopheles (60 species). The infectiousness of a mosquito after completion of sporogony remains until its death, i.e. 1-2 months.
The susceptibility to malaria of unaffected people is universally high, but individuals or ethnic groups have genetic resistance. For example, Negroid races are not susceptible to P. vivax. People with a genetic abnormality in the hemoglobin molecule (HBs - sickle cell anemia) have a relative resistance to the disease of tropical malaria, in whom malaria is milder and there is no mortality. Increased resistance to P. vivax is characterized by individuals with a genetically determined deficiency of the enzyme G-6PD (glucose-6-phosphate dehydrogenase) in erythrocytes. Newborns born to mothers with strong antimalarial immunity have natural immunity to malaria during the first 3 months of life.
In endemic areas, frequent reinfections with malaria lead to the development of high levels of acquired immunity. However, if there are no repeated infections, it is lost. Immunity to malaria is species- and strain-specific, lasting on average up to 1 year.
Epidemic process. The global spread of malaria is determined by the distribution area of the vector, the mosquito of the genus Anopheles, and the temperature factor that regulates the completion of the sporogony process. Moreover, temperature conditions more strictly limit the spread of malaria, since the minimum temperature threshold for the development of malarial plasmodium in the vector is 16 ⁰ C, which is higher than the threshold for the development of Anopheles larvae (10 ° C). Thus, the nosoarea of malaria is smaller than the range of Anopheles. Accordingly, the northern border of the malaria range in the Old World quite accurately coincides with the isotherm of more than 15 ⁰ C for 30 days a year, in the New World - with the summer isotherm of 21 ° C.
Among the socio-economic factors, the greatest influence on the formation of the nosoarea of malaria is exerted by the economic activity of the population (development of irrigated agriculture, trade, development of new lands, etc.) and migration.
Tropical malaria is mainly common in countries of the tropical and subtropical zones. Foci of four-day malaria are located in clusters in Africa, some areas of Central and South America, the Caribbean, and Southeast Asia. The distribution area of P. ovale is small and consists of the African zone and the zone located in South-West Asia and Oceania (New Guinea, Philippines, Vietnam, Thailand).
Thanks to targeted antimalarial measures, changes occurred in the structure of the nosoarea, its area decreased, and morbidity and mortality decreased. However, the most intense endemic foci of malaria remain in African countries (Senegal, Mali, Ethiopia, Nigeria), the Caribbean Sea, and in the south and southeast of Asia (India, Bangladesh, Pakistan, Vietnam, Sri Lanka).
The global nosoarea of malaria is heterogeneous in terms of endemicity, i.e., in the prevalence of malaria in a specific territory.
In accordance with the WHO classification (1950), there are 4 levels of endemic malaria depending on the value of the splenic index (SI) in children 2-9 years of age (SI - the number of persons with an enlarged spleen among those examined): hypoendemic - SI up to 10%; mesoendemia - SI 11-50%; hyperendemia SI 51-75%; holoendemia - SI above 75%. In holo- and hyperendemic territories, the reproduction of new cases occurs intensively almost all year round and the epidemic process is characterized as stable. The intensity of the reproduction of new cases of infection in meso- and hypoendemic areas is quite high in certain seasons of the year, but the epidemic process is characterized by signs of instability. With a clearly unstable epidemic process, the incidence of malaria becomes epidemic in nature, i.e., individual cases of importation of the disease or outbreaks of this infection are recorded.
The focus of malaria is a populated area with adjacent anophelogenic reservoirs. Based on the activity of the epidemic focus of malaria, the following types of outbreaks are distinguished: pseudofocus - the presence of cases of importation of the disease without the possibility of transmission of the pathogen; potential - the presence of cases of imported infection, there are conditions for transmission of the malaria pathogen; active new - the emergence of cases of local infection with transmission of the malaria pathogen, active persistent - the presence of cases of local infection for 3 years or more without interruption of transmission; inactive (recovered) - transmission of the malaria pathogen has stopped; over the past 2 years there have been no cases of local infection.
The incidence of malaria in any part of its global range is seasonal, which is associated with the biology of its vectors and the characteristics of the pathogen. The seasonality of the spread of malaria is determined by the temperature factor, which favors the mass reproduction of mosquitoes and the completion of sporogony.
The malaria transmission season is the period during which it is possible for humans to become infected with malaria through the bites of mosquitoes infected with Plasmodium that year. This period begins from the day when, due to temperature conditions, the maturation of sporozoites can be completed. Its duration in countries of temperate and subtropical climates is from 1.5 to 6-7 months. In tropical countries, transmission of the pathogen occurs almost all year round.
In endemic regions with high levels of endemic malaria, children and weakened individuals who do not have natural immunity are more likely to suffer from malaria.
The incidence of malaria in Russia at the beginning of the twentieth century. reached 3-5 million cases, three-day vivax malaria predominated among the sick. Tropical malaria was prevalent mainly in the southern regions, especially in Central Asia, where it accounted for 63-66% of the number of malaria patients. By 1960, as a result of the implementation of the state program to combat malaria, the incidence rate dropped to less than 0.1 per 100 thousand population, and tropical malaria was eliminated. Only imported cases were recorded. This situation was regarded as confirmation of the elimination of malaria as a mass disease and the transition to the next stage of malaria elimination throughout the USSR. However, active foci of malaria remained in Tajikistan, Azerbaijan, and Uzbekistan.
The malaria situation in the Russian Federation in the 90s of the twentieth century began to change, which was associated with socio-economic transformations in the country. Both the number of “imported” cases from the CIS countries and non-CIS countries, as well as the number of “local” cases of the disease, have increased. The majority of “imported” cases (up to 80%) are patients with three-day malaria, detected primarily in large cities (Moscow, St. Petersburg). In a number of territories (Moscow, Ryazan, Samara, Volgograd, Kemerovo regions, the Republic of Tatarstan and Bashkortostan) cases of local malaria have been registered.
Preventive and anti-epidemic measures.
In the Russian Federation and those countries in which the main problem in maintaining the achieved malaria prosperity has become “imported” malaria, epidemiological surveillance of malaria is of paramount importance.